The realm of healthcare is undergoing a significant transformation, thanks to the rapid advancement of technology. This article explores the various technological innovations that are reshaping healthcare delivery, improving patient outcomes, and streamlining healthcare operations. From the rise of AI in diagnostics to the integration of genomics into personalized medicine, these advancements signify a new era in medical care that is more efficient, accessible, and tailored to individual needs.
Key Takeaways
- Artificial Intelligence (AI) is revolutionizing medical diagnostics with its ability to analyze complex datasets and improve decision-making.
- Telemedicine is expanding access to healthcare by allowing patients to consult with providers remotely, overcoming geographical barriers.
- Wearable technology and the Internet of Things (IoT) are enabling continuous patient monitoring, leading to proactive healthcare management.
- Extended Reality (XR) technologies are enhancing medical training and treatment, offering immersive experiences that improve learning and patient care.
- Healthcare is modernizing legacy systems to meet current demands, ensuring that infrastructure can support the latest technological innovations.
Technological Advancements in Healthcare

The Rise of Artificial Intelligence in Medical Diagnostics
Artificial intelligence (AI) is revolutionizing the field of diagnostics by enhancing accuracy and efficiency in disease detection and diagnosis. Through machine learning algorithms and data analytics, AI-powered diagnostic tools can analyze vast amounts of medical data with unparalleled speed and precision, aiding healthcare providers in early detection of diseases and conditions.
From medical imaging interpretation to pattern recognition in laboratory tests, AI algorithms are augmenting healthcare professionals’ diagnostic capabilities, leading to faster diagnosis and more effective treatment planning. In medical imaging, AI algorithms are transforming the interpretation of radiological images, enhancing diagnostic accuracy and efficiency. By analyzing imaging data and identifying subtle abnormalities that may be missed by the human eye, AI-powered imaging solutions enable healthcare providers to make more informed diagnostic decisions and develop personalized treatment plans tailored to each patient.
AI technology is now being implemented into predictive medical diagnosis software. These tools use machine learning algorithms to analyze medical data and predict the likelihood of certain medical conditions or diseases in patients. It can assist healthcare providers in making informed decisions based on data-driven insights, improving the accuracy and efficiency of medical diagnosis and treatment.
The integration of AI and machine learning is not only aiding in diagnosis and treatment but is also playing a pivotal role in patient engagement. Remote patient monitoring and wearable devices are becoming commonplace, allowing continuous tracking of health metrics and facilitating personalized care.
Telemedicine: Bridging the Gap Between Patients and Providers
Telemedicine has emerged as a game-changer in the realm of healthcare, particularly in improving access to medical services. Through telecommunication and digital platforms, patients can now connect with healthcare providers remotely, eliminating geographical barriers and enabling timely consultations. This innovation has proven especially crucial in rural areas and underserved communities where access to healthcare facilities may be limited.
By leveraging telemedicine, healthcare providers can offer consultations and medical advice to individuals who would otherwise struggle to access timely healthcare services. In remote areas, telemedicine serves as a lifeline, ensuring that even those in the most remote locations have access to quality healthcare.
The benefits of telemedicine extend beyond just accessibility:
- Access to specialized care: Patients gain access to specialized medical expertise regardless of their location.
- Convenience and flexibility: Virtual consultations offer the ability to connect with specialists from home, without the need for travel.
As we look to the future, the implications of telemedicine’s advancements are vast, promising to further transform the healthcare landscape.
Wearable Technology and IoT: A New Era of Patient Monitoring
The integration of wearable technology and the Internet of Things (IoT) is revolutionizing patient monitoring, offering unprecedented levels of data and insights into personal health. Wearable devices such as smartwatches, fitness trackers, and health monitoring sensors are at the forefront of this transformation. These gadgets provide real-time biometric data, including heart rate, activity levels, and sleep patterns, enabling individuals to proactively manage their health.
IoT applications extend beyond wearables, incorporating smart hospital beds and sensors that detect falls or unusual movements, instantly alerting medical staff. For instance, the IntelliVue Guardian solution uses wearable biosensors and IoT connectivity to continuously monitor vital signs and send alerts for rapid response.
The rise of wearable devices and IoT in healthcare signifies a shift towards more proactive and personalized patient care. It empowers patients to actively participate in their health management while providing healthcare professionals with the tools for better decision-making and early intervention.
Here’s a glimpse of the impact of wearable technology in healthcare:
- Real-time health monitoring: Continuous tracking of vital signs and physical activity.
- Emergency response: Quick alerts and tracking in critical situations.
- Patient empowerment: Individuals can monitor their health and make informed decisions.
- Data-driven care: Healthcare providers receive timely data for improved patient outcomes.
As these technologies continue to evolve, they will further enhance patient care and the efficiency of healthcare services.
Extended Reality: Transforming Medical Training and Treatment
Extended reality (XR) technologies, encompassing augmented reality (AR), virtual reality (VR), and mixed reality (MR), are revolutionizing the healthcare industry. Clinicians are tapping into extended reality technologies for a variety of applications, from enhancing medical education to assisting in complex surgeries. The immersive nature of XR provides a rich, interactive learning environment that caters to different learning styles, making it an invaluable tool in medical training.
In the realm of treatment, XR is making strides in areas such as rehabilitation and physical therapy. AR, in particular, is being used to create engaging exercises that motivate patients and improve outcomes. Moreover, VR has shown promise in treating conditions like phobias and PTSD, with specialized centers and companies developing targeted VR therapies.
The integration of XR in healthcare is not without its challenges, but the benefits are clear. As the technology becomes more accessible and cost-effective, we can expect to see a wider adoption in primary care and other specialties. The table below highlights some of the key areas where XR is currently being applied in healthcare:
| XR Application | Description |
|---|---|
| Medical Education | Simulated environments for training |
| Surgery Assistance | Real-time guidance during procedures |
| Rehabilitation | Interactive exercises for recovery |
| Treatment of Phobias | VR therapy for specific conditions |
The potential of extended reality to enhance patient care and medical education is immense. As we continue to explore and expand its applications, XR stands to become a cornerstone in the future of healthcare.
Modernizing Legacy Systems to Meet Current Healthcare Demands
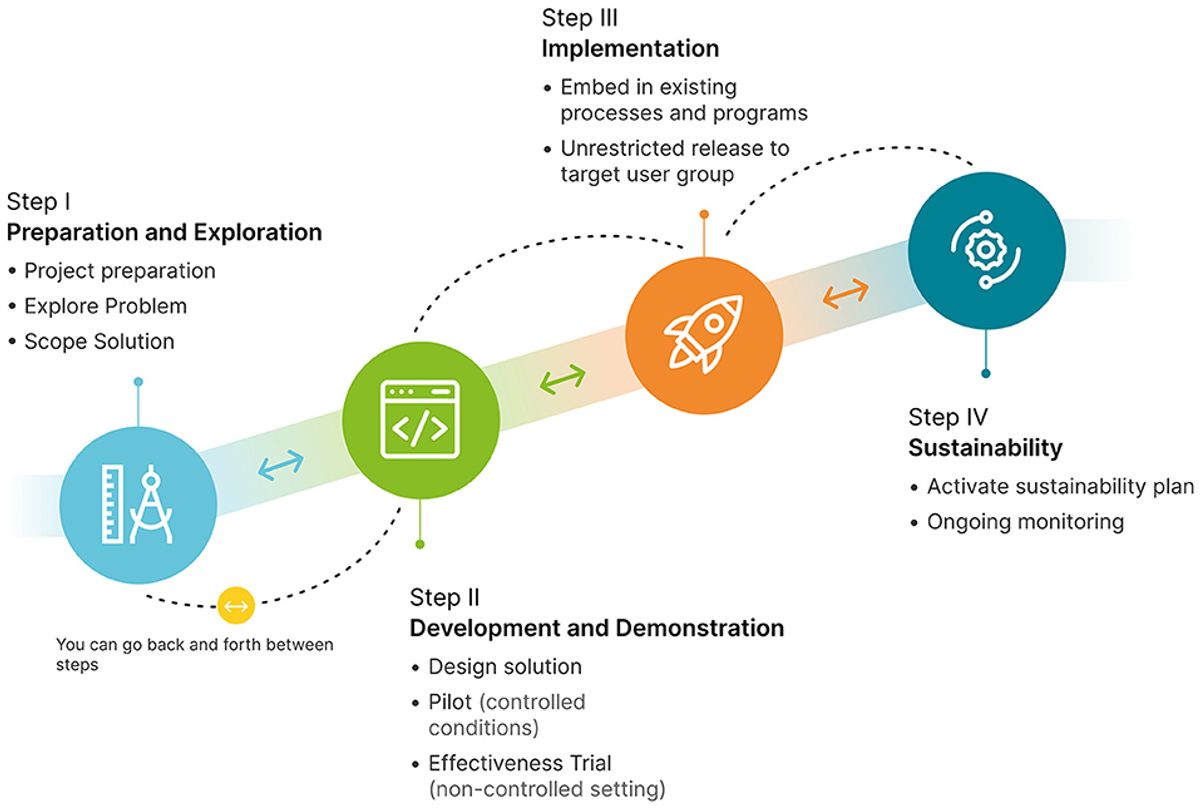
The healthcare industry is currently facing the challenge of modernizing legacy systems to better meet market demands and enhance patient care. Proactive legacy system modernization involves not only upgrading outdated software but also implementing new technologies that improve security, interoperability, and user experience.
Modernization efforts often include:
- Migrating to advanced healthcare software platforms
- Transitioning to modern operating systems
- Re-engineering software to meet specific needs
Establishing a clear strategic direction and instigating a cultural mindset shift are crucial for successful modernization.
With 73% of health systems using medical equipment on legacy operating systems, the urgency to modernize is underscored by the increasing frequency of security breaches and rising patient expectations. By addressing these challenges, healthcare organizations can ensure the delivery of more efficient and secure patient care.
Personalized Medicine and Genomics
Tailoring Treatments with Genetic Profiling
The advent of personalized medicine has ushered in a new paradigm in healthcare, where treatments are tailored to the individual’s genetic makeup. This approach not only enhances the efficacy of treatments but also minimizes the risk of adverse reactions. By analyzing a patient’s genetic profile, healthcare providers can identify the most effective interventions for preventing and treating diseases.
Precision medicine is at the forefront of this revolution, enabling the customization of healthcare, with decisions and treatments being tailored to individual patients. This shift from a one-size-fits-all methodology to a more personalized approach is a significant leap forward in medical science.
The impact of genetic profiling on treatment plans can be summarized as follows:
- Identification of genetic risks: Pinpointing individuals at higher risk of certain diseases.
- Early intervention: Facilitating preventive measures and early treatments.
- Customized therapies: Developing treatment plans that are more likely to succeed based on genetic information.
- Reduced side-effects: Lowering the chances of adverse drug reactions by avoiding medications that are incompatible with the patient’s genetic profile.
The Impact of Big Data on Personalized Care Plans
The integration of big data in healthcare is revolutionizing the way personalized care plans are developed and implemented. By leveraging patient-specific data, healthcare providers can create highly tailored treatment plans that address the unique needs of each individual.
For instance, the use of customized, patient-centric analytics is on the rise. Traditional one-size-fits-all tools are being replaced with solutions that provide insights specific to individual healthcare scenarios. This not only enhances patient care but also boosts operational efficiency.
Remote monitoring technology is a prime example of big data’s role in personalization. It enables the creation of care plans that are truly aligned with a patient’s health conditions and lifestyle, leading to better health outcomes and increased patient satisfaction.
The era of personalized healthcare is upon us, with patient-generated health data (PGHD) and genomics paving the way for treatments that are fine-tuned to each patient’s genetic makeup, lifestyle, and preferences. The table below illustrates the shift from generic to personalized analytics in healthcare:
| Year | Generic Analytics Usage | Personalized Analytics Adoption |
|---|---|---|
| 2020 | High | Low |
| 2024 | Decreasing | Increasing |
Embracing this data-driven approach is not just about technology; it’s about a cultural shift in data governance that prioritizes the individual’s health journey.
Advancements in Pharmacogenomics for Drug Development
Pharmacogenomics is revolutionizing the way we approach drug development, offering a path to more personalized and effective treatments. By understanding an individual’s genetic makeup, medical professionals can predict responses to medications, enhancing efficacy and reducing adverse effects. This approach is particularly promising in addressing complex challenges such as the opiate crisis in America.
Recent collaborations in the field have demonstrated the power of combining traditional methods with cutting-edge technologies. For example, a partnership between Accenture Labs, 1QBit, and Biogen utilized quantum-enabled applications to analyze molecular data, resulting in significant time and cost savings for drug development.
The integration of patient-generated health data with genomic insights is paving the way for truly personalized healthcare. Treatments are now being tailored to individual genetic profiles, taking into account lifestyle and personal preferences.
The table below summarizes some of the key benefits of pharmacogenomics in drug development:
| Benefit | Description |
|---|---|
| Efficacy | Tailored drug regimens increase the likelihood of treatment success. |
| Safety | Reduced risk of adverse drug reactions by considering genetic factors. |
| Cost | Potential savings through more efficient drug development processes. |
| Time | Faster time to market for new drugs by streamlining research and trials. |
Integrating Genomic Data into Electronic Health Records
The integration of genomic data into electronic health records (EHRs) is a transformative step in personalized medicine. It enables healthcare providers to tailor treatments based on a patient’s genetic profile, potentially improving outcomes and reducing adverse reactions. This integration also supports the shift towards precision medicine, where genetic information plays a crucial role in diagnosing and managing diseases.
The seamless integration of patient data, including genomic information, into EHRs enhances care coordination and reduces the risk of errors associated with manual record-keeping.
However, there are challenges to overcome, such as ensuring the privacy and security of sensitive genetic information and establishing interoperability among diverse EHR systems. Educating patients and healthcare professionals about the benefits and use of genomic data within EHRs is also essential.
- Educating patients to use wearables and other health technologies
- Overcoming trust issues in sharing medical data
- Ensuring privacy and security of genetic information
- Establishing interoperability among EHR systems
Improving Patient Engagement and Communication
Enhancing Patient-Provider Interactions with Digital Tools
In the ever-evolving landscape of healthcare, effective communication is pivotal for patient engagement. Secure messaging platforms are now a staple, enabling real-time dialogue between patients and their care teams. The advent of virtual health assistants and chatbots has further revolutionized this space, offering immediate responses to routine inquiries and fostering a supportive network.
Digital tools are reshaping the healthcare experience, making it more personalized and accessible. These innovations include telemedicine for virtual consultations, wearable technology for health tracking, and the use of artificial intelligence in diagnostics. The integration of these tools into healthcare practices is not just a trend but a transformative force.
As healthcare continues to advance, the digitalization of patient engagement is creating new avenues for care that are both efficient and patient-centric. The synergy between patients and providers is strengthened, transcending the traditional boundaries of clinics and hospitals.
The table below highlights the impact of digital tools on patient engagement:
| Digital Tool | Function | Impact on Patient Engagement |
|---|---|---|
| Secure Messaging | Real-time communication | Enhances connectivity |
| Virtual Health Assistants | Instant query response | Increases accessibility |
| Wearable Technology | Health tracking | Empowers patients |
| Telemedicine | Virtual consultations | Improves outcomes |
Mobile Health Apps and Their Role in Patient Empowerment
Mobile health (mHealth) apps are revolutionizing the way individuals engage with their healthcare. By harnessing the power of mobile devices, these apps provide patients with unprecedented access to health information and services, fostering a more active role in their own care. Patient empowerment is at the forefront of this transformation, as users gain greater control over their health data and become active participants in their healthcare journey.
The impact of mHealth apps extends beyond mere access to information; they also offer innovative ways to encourage patient involvement. For instance, some apps incentivize engagement through rewards, effectively promoting consistent use and data contribution. This not only benefits the individual by fostering a habit of health awareness but also enriches the overall quality of healthcare data available.
Patient education is a critical aspect of empowerment. The integration of gamification techniques in mHealth apps makes learning about health conditions more interactive and enjoyable. As patients become better informed, they are equipped to make decisions that positively influence their health outcomes.
Furthermore, the use of health monitoring sensors within these apps allows patients to track their well-being in real-time. This immediate feedback loop empowers patients to manage their health proactively, adjusting their lifestyle and treatment plans as needed to maintain optimal health.
The Importance of Health Literacy in Patient Education
Health literacy is pivotal in enabling patients to grasp complex medical information and make informed decisions. Educating patients about their health conditions is not just about conveying information; it’s about ensuring comprehension and application in daily life. Innovative approaches, such as gamification, are making learning more engaging and interactive, fostering a shift from passive care recipients to active participants in health management.
Healthcare professionals play a critical role in this educational process. Training programs are now emphasizing empathetic communication and patient-centered care. Addressing burnout among providers is also essential to maintain the quality of patient education.
Patient portals are a testament to the power of health literacy. These platforms allow patients to:
- Access personal health information
- Schedule appointments
- Refill prescriptions
- Communicate with healthcare providers
By engaging with their health data, patients are better equipped to participate in shared decision-making.
Empowerment through knowledge is the cornerstone of modern patient education. It transforms the patient-provider relationship and leads to improved health outcomes.
Social Media as a Platform for Health Awareness and Support
Social media platforms have become pivotal in disseminating health information and fostering community support. Patients increasingly use platforms like Facebook, Instagram, and Twitter to share their experiences, seek advice, and access health-related content. This trend has given rise to a new dimension of e-health data that is valuable for healthcare businesses.
Healthcare providers are recognizing the importance of engaging with patients through these digital channels. By doing so, they can enhance the patient experience and provide support beyond the clinical setting. The table below illustrates the various ways social media is being utilized in healthcare:
| Platform | Use Case |
|---|---|
| Patient support groups | |
| Health awareness campaigns | |
| Real-time health updates |
The integration of social media in healthcare is not without challenges. Privacy concerns and the need for accurate information dissemination are paramount. However, the potential for improved patient engagement and community support is significant.
As we move forward, it is clear that social media will continue to play a crucial role in health awareness and support. Collaborative efforts between healthcare providers, patients, and community organizations are essential to leverage these platforms effectively and promote holistic well-being.
Data Security and Privacy in the Digital Age

Protecting Patient Information in an Era of Cyber Threats
In the digital age, healthcare organizations are intensifying their cybersecurity efforts to safeguard patient information. The rise in cyber threats has made data security a top priority, with a focus on preventing disruptions to patient care and preserving the trust between patients and providers.
- Trend #6: Data security is now a critical priority for healthcare providers.
- In 2024, significant investments are being made in cybersecurity measures.
- Compliance with data protection regulations is foundational for maintaining patient trust.
Striking the right balance between technological innovation and data security is a key challenge in the healthcare industry.
According to IBM, the period between March 2021 and March 2022 saw 550 organizations worldwide suffer data breaches. Notably, in 2023, Truepill experienced a massive data breach impacting over 2.3 million individuals, highlighting the urgency for strengthened security measures.
The Role of Blockchain in Ensuring Data Integrity
Blockchain technology offers a secure and transparent way to manage health records and transactions. It represents a paradigm shift in how healthcare data is shared and stored, ensuring that each transaction is encrypted and immutable. This technology is particularly promising for enhancing security and reducing the risks for data breaches, which are a growing concern in the healthcare industry.
Blockchain’s distributed ledger technology allows for a tamper-proof record of patient data and transactions, which is crucial for maintaining data integrity.
Healthcare organizations are beginning to pilot blockchain projects to explore its potential in various areas, including health information exchange and supply chain management. The ability to securely manage and share data can lead to more proactive and preventive care, as anonymized patient data can be exchanged across hospitals to identify early symptoms and reduce healthcare costs.
However, the adoption of blockchain in healthcare faces challenges such as regulatory compliance and the establishment of interoperability standards. Despite these hurdles, the promise of blockchain to safeguard patient information and streamline healthcare processes continues to drive interest and investment in this technology.
Regulatory Compliance and Ethical Considerations
In the realm of healthcare, compliance with regulations such as HIPAA in the United States and GDPR in the European Union is not just a legal formality but a cornerstone of patient trust and safety. The integration of technology, especially AI, into healthcare heightens the importance of safeguarding patient data and ensuring privacy.
Healthcare organizations are increasingly investing in robust cybersecurity measures to protect sensitive health information. This is crucial for maintaining patient trust and adhering to ethical standards. The table below outlines key areas of focus for regulatory compliance in healthcare technology:
| Area of Focus | Description |
|---|---|
| Patient Safety | Ensuring technology does not compromise patient well-being. |
| Data Privacy | Protecting sensitive patient information from unauthorized access. |
| Ethical Standards | Upholding ethical considerations in the use of AI and data processing. |
Striking the right balance between technological innovation and data security is a key challenge that healthcare providers must navigate. Tailored solutions may be necessary when existing data infrastructure does not meet the stringent requirements for ePHI exchange or when specialized video conferencing software is required.
As the landscape of healthcare technology evolves, regulatory compliance remains as critical as the technological advancements themselves. It is imperative for healthcare providers to implement and continuously update security measures to prevent breaches and misuse of patient data.
Implementing Robust Data Governance Frameworks
In the realm of healthcare, data governance is pivotal for ensuring the integrity, confidentiality, and availability of patient information. A robust data governance framework encompasses a set of policies, procedures, and standards that guide the collection, management, and use of health data.
Establishing a clear strategic direction and instigating a cultural mindset shift are essential for modernizing healthcare systems and improving coordination through centralized and shared data.
Key components of a successful data governance framework include:
- Data Quality Management
- Data Access and Permissions
- Compliance with Regulatory Standards
- Risk Management Strategies
- Performance Monitoring and Improvement
By prioritizing data security, healthcare providers can build a business case for data governance, highlighting its role in protecting patient information and enabling better healthcare outcomes.
Interoperability and Health Information Exchange

The Challenges and Solutions for Seamless Data Sharing
The healthcare industry is at a crossroads when it comes to data sharing. On one hand, the potential for improved patient outcomes through better coordination is immense. Electronic Health Records (EHRs) are at the forefront of this transformation, promising seamless information sharing across different healthcare facilities. However, the journey is fraught with challenges, particularly around data security and privacy.
- Challenges:
- Diverse EHR systems with incompatible formats
- Concerns over patient privacy and consent
- Regulatory hurdles and varying standards
- Risk of data breaches and cyber-attacks
- Solutions:
- Adoption of universal data exchange standards
- Implementation of robust cybersecurity measures
- Leveraging blockchain for enhanced data integrity
- Encouraging transparency and patient control over data
The integration of blockchain technology is seen by many as a pivotal solution to these challenges, offering a secure and immutable ledger for health data transactions. This innovation could be the key to unlocking the full potential of data sharing in healthcare, while also addressing the critical issue of data security.
Striking the right balance between innovation and security is essential. As we move forward, the focus must be on developing frameworks that not only facilitate data sharing but also protect the sensitive information of patients and healthcare providers.
EHR Systems and the Quest for Nationwide Interoperability
The quest for nationwide interoperability in electronic health records (EHRs) is a pivotal aspect of modern healthcare. Interoperability remains a challenge, but there is a concerted effort to overcome the barriers that prevent seamless information exchange. The goal is to enable healthcare providers to access comprehensive patient records, regardless of where the patient received care, which is essential for coordinated and patient-centric care.
Interoperable EHR systems are crucial for facilitating continuity of care and enhancing the patient experience. To achieve this, stakeholders across the healthcare ecosystem must collaborate to address standardization and interoperability challenges. The integration of EHR/EMR information with data from IoT sources and internal hospital systems is a complex task that requires a multifaceted approach.
Modernization efforts in healthcare should focus on enabling seamless data exchange and interoperability with other systems. This includes not only EHRs but also laboratory information systems and other healthcare technologies.
The table below outlines some of the key challenges and solutions associated with achieving nationwide interoperability in EHR systems:
| Challenge | Solution |
|---|---|
| Standardization | Adoption of common data standards |
| Data Sharing | Implementation of health information exchanges |
| Privacy & Security | Robust data governance frameworks |
| Technology Integration | Upgrading legacy systems |
As we move forward, the examples set by successful interoperability initiatives will serve as a guide for ongoing efforts to connect healthcare systems across the nation.
Fostering Collaboration Through Health Information Networks
Health information networks are pivotal in achieving interoperability, allowing for the secure and efficient exchange of patient data among different healthcare entities. The goal is to create a cohesive healthcare environment where information flows freely, supporting coordinated and continuous care.
- Standardization of data formats and protocols, such as FHIR, is crucial.
- Participation in health information networks by healthcare organizations is on the rise.
- These networks alleviate administrative burdens, enabling healthcare professionals to concentrate on patient care.
By fostering collaboration through health information networks, the healthcare industry is taking a significant step towards a more integrated and patient-centered approach to care delivery.
Challenges remain, however, including the need for widespread adoption and the harmonization of standards. Stakeholders must work together to overcome these barriers and realize the full potential of interoperable health information exchange.
The Future of Health Data Exchange and Patient-Centered Care
As we look towards the future, the integration of health data exchange into patient-centered care is becoming increasingly important. Propelled by technological innovations and the changing needs of patients, there’s a noticeable pivot towards care centered on the patient, focusing on outcomes. Interoperability between healthcare systems and devices is crucial to make patient data accessible and usable across various platforms. In 2024, the emphasis on health information exchange will be more pronounced, with healthcare organizations adopting standards like FHIR and participating in health information networks to facilitate better care coordination.
The seamless integration of health data across platforms is not just a technical challenge but a step towards a more empathetic and efficient healthcare system.
Challenges such as standardization and the need for collaborative efforts from stakeholders are recognized as essential for delivering coordinated and patient-centric care. Electronic health records (EHRs) play a central role in this evolution. However, the journey towards interoperability and integration into EHRs will require overcoming hurdles like educating patients on the use of wearables and addressing trust issues related to sharing medical data through remote monitoring devices.
Conclusion
As we have explored throughout this article, the horizon of healthcare technology is ever-expanding, with innovations like AI, telemedicine, and wearable devices leading the charge in transforming patient care. These advancements not only improve the efficiency and accessibility of healthcare services but also empower patients to take an active role in managing their health. The integration of technology in healthcare is a continuous journey, with each step forward opening new possibilities for better health outcomes and a more resilient healthcare system. While challenges such as data security and the need for improved interoperability remain, the potential benefits are immense. As we look to the future, it is clear that the symbiosis of technology and healthcare will continue to evolve, offering hope for a healthier world for all.
Frequently Asked Questions
What are the key innovations driving digital healthcare?
Key innovations in digital healthcare include artificial intelligence for diagnostics, telemedicine, wearable technology, electronic health records, remote monitoring technology, and incremental improvements in healthcare administration and operations.
How does telemedicine enhance patient care?
Telemedicine enhances patient care by providing remote access to medical services, removing geographical barriers, facilitating timely consultations, and making healthcare more accessible and convenient for patients.
What role does artificial intelligence play in healthcare?
Artificial intelligence plays a critical role in healthcare by aiding in medical diagnostics, assisting with surgeries, developing new pharmaceuticals, and improving communication with patients. It is also instrumental in analyzing large datasets for better clinical decision-making.
How are wearable technologies transforming patient monitoring?
Wearable technologies and the Internet of Things (IoT) are transforming patient monitoring by enabling continuous tracking of health metrics, providing real-time data to healthcare providers, and empowering patients to manage their own health.
What is the significance of data security in healthcare?
Data security is paramount in healthcare to protect sensitive patient information from cyber threats, ensure privacy, maintain trust, and comply with regulatory requirements. Technologies like blockchain are being explored to enhance data integrity and security.
What challenges does interoperability present in healthcare, and how are they being addressed?
Interoperability challenges in healthcare include the seamless sharing of data across different systems and providers. Solutions involve the development of standards, fostering health information networks, and the implementation of robust health information exchange systems to enable patient-centered care.





